Featured Legislative & Regulatory Positions
See all Positions
AMCP opposes government regulation of drug pricing because of the potential for unintended consequences and supports the elimination of barriers to competition to bring down the high cost of prescription drugs.

The Academy of Managed Care Pharmacy (AMCP) supports scientifically sound research that compares the effectiveness and value of prescription drugs, as well as research aimed at tailoring treatment options to individual patients’ needs.

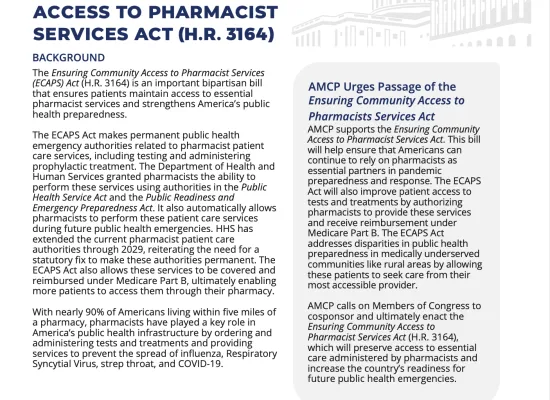
AMCP supports the recognition of pharmacists as providers. When pharmacists are recognized as provider members of the health care team, patient outcomes improve, and patients report higher rates of satisfaction while overall health care costs are reduced. Recognized provider status would allow pharmacists to be reimbursed for providing health care services to patients. In a survey conducted in 2023 commissioned by Wolters Kluwer Health, 58% of Americans agreed that they are more likely to seek non-emergency medical care from a pharmacist.
Featured Resources
See More Resources

Regulatory Updates
Letters, Statements, and Analysis
See All Letters, Statements, & Analysis
In Kennedy v. Braidwood Management, Inc., the plaintiffs challenged the constitutionality of the USPSTF, arguing that USPSTF members should be considered “principal officers” under the Appointments Clause and, therefore, must be appointed by the President and confirmed by the Senate.

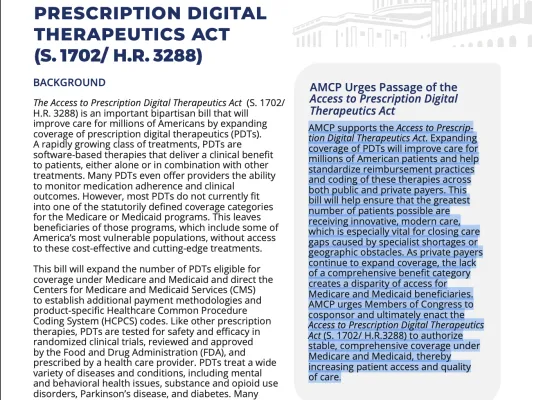
As CMS explores strategies to increase the adoption of digital health tools, AMCP urges CMS to support broader coverage of prescription digital therapeutics (PDTs) under Medicare and Medicaid. PDTs represent an emerging class of software-based treatments that deliver clinically validated therapeutic benefits, either independently or in combination with other interventions. These products can play a transformative role in improving access, especially for patients with behavioral health conditions or chronic diseases.

Following House passage of congressional Republican’s budget reconciliation package, the One Big, Beautiful Bill Act (H.R. 1), Senate Republicans took to their respective committees to provide edits and changes to the massive tax-cut, border security, energy reform, and health care package.